In this paper, we present results from an initial evaluation of the national respiratory toolkit for Wales, concentrating on the impact of this intervention on self-reported markers of asthma control. The main findings are that for those who used the app there were improvements in good asthma control as evidenced by a self-reported RCP3Q score of zero as well as a reduction in reliever inhaler usage. When we compared the RCP3Q responses from the same users after one year, we found that there were greater improvements in those who moved from poor, or sub-optimal control to better control compared to those whose control worsened, but 50% showed no change. The improvements were significant in those from the most deprived 30% and 30–50%, but not in the least deprived 50%. This finding is of significant interest given the considerable concerns about health inequality and the uptake of digital solutions.
There has been considerable interest in developing digital solutions for people with asthma partly as a result of the findings of poor basic care for people with asthma from audits such as the National Respiratory Audit Program (NRAP) led by the RCP. In a rapidly expanding field, an early systematic review of the literature on the use of mobile applications to support self-management for people with asthma from 2017 showed improved asthma control but varied clinical effectiveness of different apps17. A more recent Cochrane review of digital interventions to improve adherence to maintenance medication in asthma showed that digital interventions were likely to improve adherence, asthma control and quality of life and may even reduce exacerbations18. The World Health Organisation advocates digital health technologies to advance population health19 and digital support tools have been shown to improve blood pressure control20. Given this evidence-based support for digital interventions, and with the very poor outcomes from the primary care RCP respiratory audit in Wales, it seemed logical to adopt a digital solution to support patients with their self-management. The major difficulty was in achieving adoption of this approach at a national level. We had previously implemented a dynamic guideline nationally in Wales during COVID rapidly gaining more than 13,000 healthcare professional (HCP) signups to the platform10. This same platform was used to deliver webinars about the asthma and other apps to a wide audience of HCP to prepare and inform them about this intervention.
One of the strengths of this study, is that it is a national approach. Every GP practice in Wales has people with asthma on the app with a median number of 21, but the best performing practice had 246 app registrants. Moreover, 88% of people with asthma are introduced to the app by their HCP, indicating that the apps are held to be of value within the health ecosystem. The results represent a ‘real world’ approach, outside the controlled confines of a research environment. It is not known what is the optimum frequency to use digital support tools, but we suspect that people with asthma use them when they need them, and that varies greatly from patient to patient.
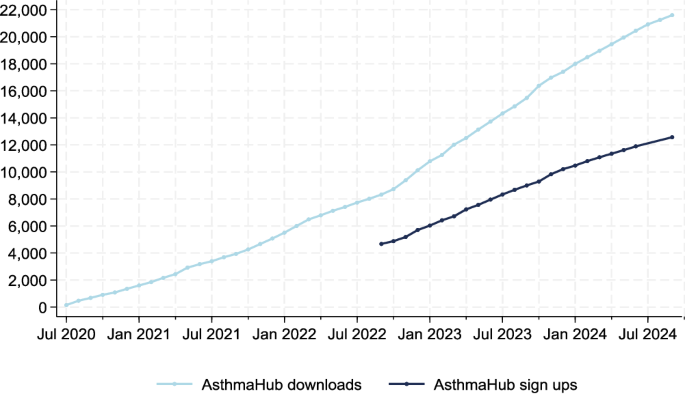
There are many limitations to this study. Whist we have 12567 adults with asthma signed up to the app by September 2024, that represents only approximately 5% of all adults with asthma in Wales. Nevertheless, we note there is a continual linear increase in app signatories over time, without payment incentives or government directives to support adoption and we have engagement from all primary care practices. Indeed, it is well appreciated within implementation science literature that adoption of new interventions takes time, with one study suggesting that it takes on average 17 years for adoption of new research into routine clinical practice21. We note that 57.8% of patients who download the app go on to register, and of those who register, half do not use it at all. The reasons behind this are unclear, but we could postulate various explanations including that this group was better controlled and did not see a need for use, app ‘fatigue’, since people tend to have many apps but only use a small number regularly or perhaps that people agreed to download to show good intentions to their HCW, but with no intention of using it. Of interest is the finding that 52.2% of people who downloaded the NHS England app subsequently went on to register, despite the fact that this app provided crucial functions during COVID, such as demonstrating a user’s vaccination status22. The factors influencing behaviours around adoption of digital solutions such as apps will likely be a focus of future research among behavioural psychologists. We would hope that future developments in the app functions, including an ‘export’ function that allows relevant aspects of a person’s asthma control over the year such as requirements for prednisolone, hospital admissions and RCP score to be viewed by a HCP as part of an asthma annual review will increase uptake and engagement with the app. Another major limitation is that the results that we have described are patient responses and are not independently validated. However, what we have collected are patient recorded outcome measures (PROMS). PROMS have a long-established role in shaping health services to be responsive to patient feedback23,24,25, have been routinely embedded across a range of specialities, and lie at the heart of understanding value-based outcomes26. Although the PROMS that we have recorded are generated directly by the patients, rather than through questionnaires administered in healthcare settings, this may be a more appropriate approach for chronic conditions with fluctuating impacts like asthma.
Another limitation is that we only have responses on the 1591 users that had completed the asthma checker requests for four months or more, representing 12.7% of all app registrants. This likely reflects to some degree differences in asthma severity and control as well as variable engagement with the digital solution. In addition, we cannot exclude the fact that regression towards the mean may be a factor in the observed differences over four months or more of app usage, since those with more troublesome asthma would be more likely to engage with the app. We noted that the demographics of the asthma checker responders showed that those that engaged with the app were slightly older, and more came from less deprived areas than those of the asthma app registrants as a whole. However, registrants from more deprived areas seemed to benefit more, in terms of greater improvements in RCP3Q scores. Lastly, whilst we have collected and analysed data on some of the asthma checker responses, we have not included important metrics such as self-reported prednisolone courses, or emergency department attendances for asthma. We report here on an initial evaluation, and believe that this is too soon to evaluate the latter data.
In this study, we have implemented a digital solution for people with asthma in Wales without mandate or incentive. We note improvements as indicated by PROMS across a number of important metrics of asthma care, including the RCP3Q responses and reductions in reliever use for those that use the app. We noted greater engagement with the app for those from less deprived areas, but a greater improvement for those from more deprived areas, offering hope for the potential of digital solutions to reduce health inequalities27. These finding support our contention that helping patients to better manage their condition improves health outcomes.
link